Bronchiectasis is a chronic lung condition that can have a profound impact on a person's quality of life. Understanding the intricacies of bronchiectasis can be overwhelming, especially when we consider its many causes and varying symptoms.
As we delve into the root causes, symptoms, and treatment options, it's crucial to be equipped with accurate knowledge, especially in an age where heart and pulmonary diseases stand as leading health concerns. Let's take a close look at bronchiectasis and learn what you can do to support your cardiopulmonary health.
What Is Bronchiectasis?
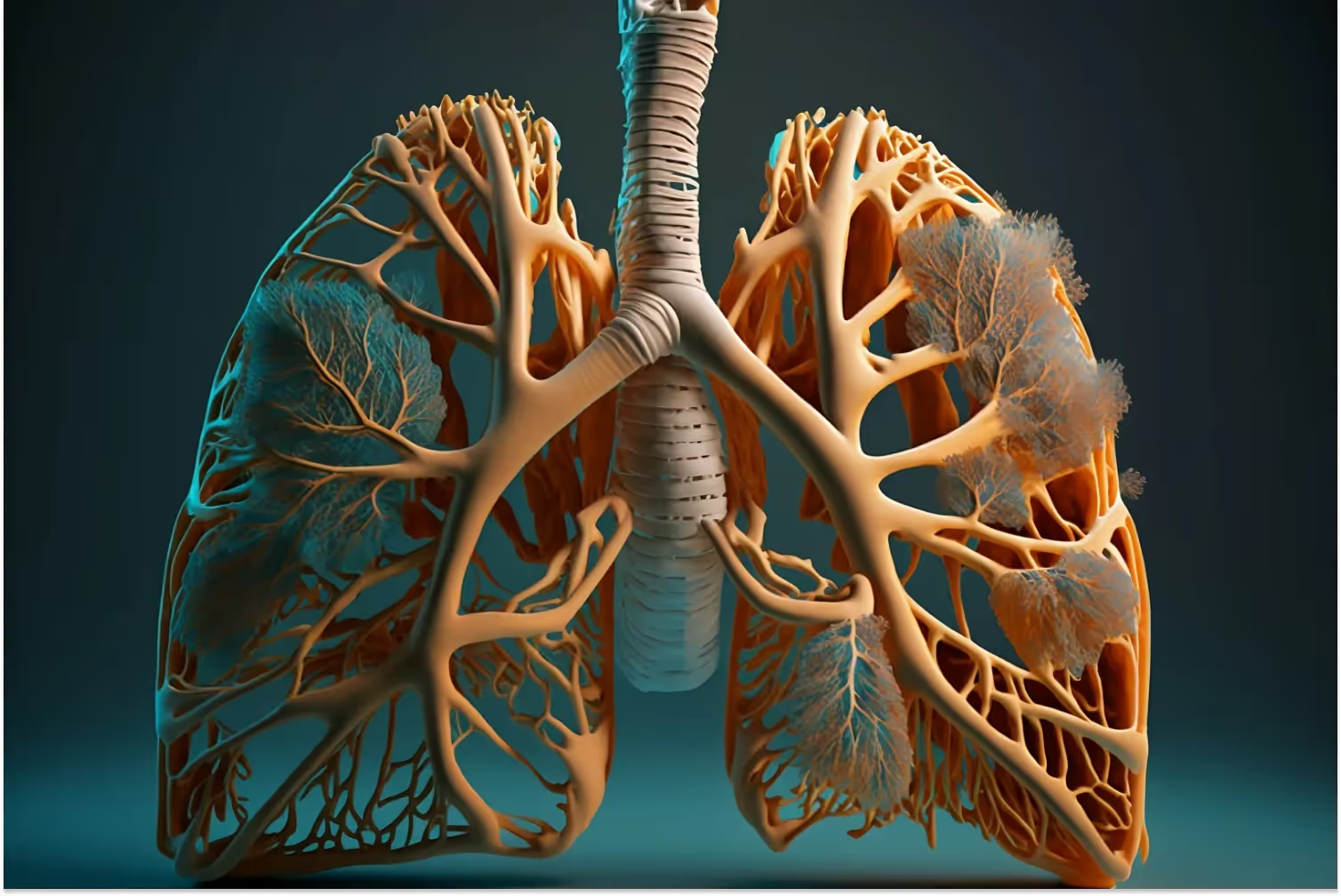
Bronchiectasis is a chronic lung condition characterized by the irreversible widening and damage of the bronchi, the airways that convey air from the trachea into the lungs. This damage often results from an infection or other condition that injures the walls of the bronchi, leading to a build-up of mucus and phlegm.
Over time, this build-up can result in further lung infections, creating a vicious cycle. Such a state can reduce the lungs' ability to move air in and out, leading to symptoms like shortness of breath and chronic coughing.
What Are the Symptoms of Bronchiectasis?
The symptoms of bronchiectasis can vary from person to person. Common symptoms include a persistent cough that produces clear mucus or sputum, shortness of breath, and chest pain. Some may experience flare-ups where symptoms become notably worse, almost resembling exacerbations of COPD (chronic obstructive pulmonary disease).
Other symptoms can include weight loss, fatigue, and, in severe cases, clubbing of the fingers and toes — a result of reduced oxygen in the blood. It's essential to be attentive to these signs, as recognizing them early can lead to more effective management and improved lung health.
How Is Cystic Fibrosis Related to Bronchiectasis?
Cystic fibrosis (CF) and bronchiectasis are both lung conditions, but they are distinctly different. However, understanding the relationship between the two is crucial for effective diagnosis and treatment.
Cystic fibrosis is a genetic disorder that results in the production of thick and sticky mucus. This mucus can clog the bronchi, which are the airways in the lungs, leading to persistent bacterial infections and inflammation.
Over time, the frequent infections and the body's inflammatory response damage the bronchi's walls. This damage can then function as an underlying cause of bronchiectasis. In simpler terms, bronchiectasis can be a direct consequence of untreated or inadequately managed cystic fibrosis.
Bronchiectasis tends to occur in young patients with CF, making early diagnosis and management essential. Recognizing the early signs of bronchiectasis, such as persistent cough, increased sputum production, and frequent lung infections, can be indicative of the need for more aggressive CF management.
What Other Health Conditions Can Lead to Bronchiectasis?
While bronchiectasis can develop after recurrent lung infections or due to underlying conditions like cystic fibrosis, several other health conditions can also act as a catalyst.
Rheumatoid arthritis, for instance, is primarily a joint disease but can have pulmonary manifestations that lead to bronchiectasis. Similarly, alpha-1 antitrypsin deficiency, a genetic disorder, can cause lung damage and subsequent bronchiectasis due to the lack of a protein that protects the lungs. Inflammatory bowel disease has also been linked to bronchiectasis, although the exact mechanism remains an area of ongoing research.
Allergic bronchopulmonary aspergillosis (ABPA), a condition caused by an allergic reaction to a specific fungus, can result in bronchiectasis if untreated. Primary ciliary dyskinesia, a congenital condition, causes cilia in the lungs to malfunction, preventing them from clearing out mucus efficiently, thus paving the way for bronchiectasis.
How Is Bronchiectasis Diagnosed?
Diagnosing bronchiectasis involves a combination of clinical evaluation and imaging tests. Symptoms such as chronic coughing up of sputum, shortness of breath, and recurrent lung infections raise suspicion. Imaging modalities like a chest X-ray can provide preliminary insights, but a CT scan remains the gold standard, offering detailed images of the bronchi.
In certain cases, bronchoscopy might be utilized. This procedure involves threading a tiny camera into the bronchi to visualize any abnormalities directly. Sputum cultures can help identify specific bacterial infections and lung function tests assess the severity of the condition and gauge overall lung health.
How Can Bronchiectasis Be Treated?
Treatment of bronchiectasis aims at managing symptoms, preventing exacerbations, and enhancing the patient's quality of life. One of the foremost strategies is expectorants, which are medications that help clear mucus from the bronchi. Bronchodilators aid in widening the airways, making it easier to breathe. For bacterial infections, antibiotics are prescribed.
Physical therapy, especially postural drainage techniques, is beneficial in assisting mucus clearance. Vaccinations, especially against the flu and pneumococcal pneumonia, can prevent lung infections, thereby reducing the risk of exacerbations. In severe cases where other treatments don’t provide relief, surgery may be an option, especially for localized bronchiectasis.

How Can Carda Health Support Those With Bronchiectasis?
Bronchiectasis can be a debilitating lung condition, often requiring comprehensive care and a multidisciplinary approach. With modern advancements in healthcare, virtual health platforms like Carda Health are bridging gaps in traditional care pathways, making it easier for patients to access specialized care right from the comfort of their homes.
Carda Health's virtual rehabilitation program is designed with the patient's needs in mind. For those with bronchiectasis, supporting lung function and maintaining optimal lung health are key.
Carda's personalized rehabilitation plans prioritize breathing exercises and techniques that can assist in clearing mucus from the bronchi, thus reducing the risk of infections and flare-ups. Incorporating exercises that focus on strengthening the respiratory muscles can further enhance lung function and stamina.
We also dedicate ourselves to education. Patients are educated about the importance of timely vaccinations, recognizing early signs of exacerbations, and understanding when to seek medical intervention. This empowers our patients, giving them the tools and knowledge to better manage their condition.
Our platform offers regular follow-ups and check-ins, ensuring that any potential issues are identified and addressed promptly. This continuity of care, combined with the convenience of virtual healthcare, ensures that our patients with bronchiectasis receive comprehensive, consistent, and tailored care that can significantly improve their quality of life.
The Bottom Line
Bronchiectasis, with its persistent cough, sputum production, and recurrent lung infections, can profoundly impact an individual's quality of life. However, understanding its causes, recognizing symptoms early, and seeking appropriate diagnosis and treatment are pivotal in managing the disease.
Modern treatment modalities, both pharmacological and physical, can alleviate symptoms and reduce the risk of exacerbations. And with innovative healthcare platforms like Carda Health, patients now have an added layer of support.
The future of managing bronchiectasis looks promising, with advancements in healthcare technology and a patient-centric approach leading the way. To learn more about healthcare and to equip yourself with knowledge about your health condition, head on over to our blog.
Sources:
COPD - Symptoms and causes | Mayo Clinic
About Cystic Fibrosis | Cystic Fibrosis Foundation

.avif)