The modern medical landscape is full of innovations and technologies that are designed to better the lives of patients around the world. One such advancement is the use of hernia mesh in surgeries to address the often debilitating condition of hernias.
But what exactly is hernia mesh made of? And how does it function within the body? In this guide, we delve deep into the intricacies of hernia mesh, offering insights into its materials, construction, and applications in medical procedures.
What Is Hernia Mesh?
Hernia mesh is a medical device widely used during hernia repair surgeries. A hernia occurs when an organ, typically a portion of the intestine, pushes through the muscle or tissue meant to hold it in place. To mitigate this, surgeons utilize hernia mesh to provide added support to the weakened or damaged tissue.
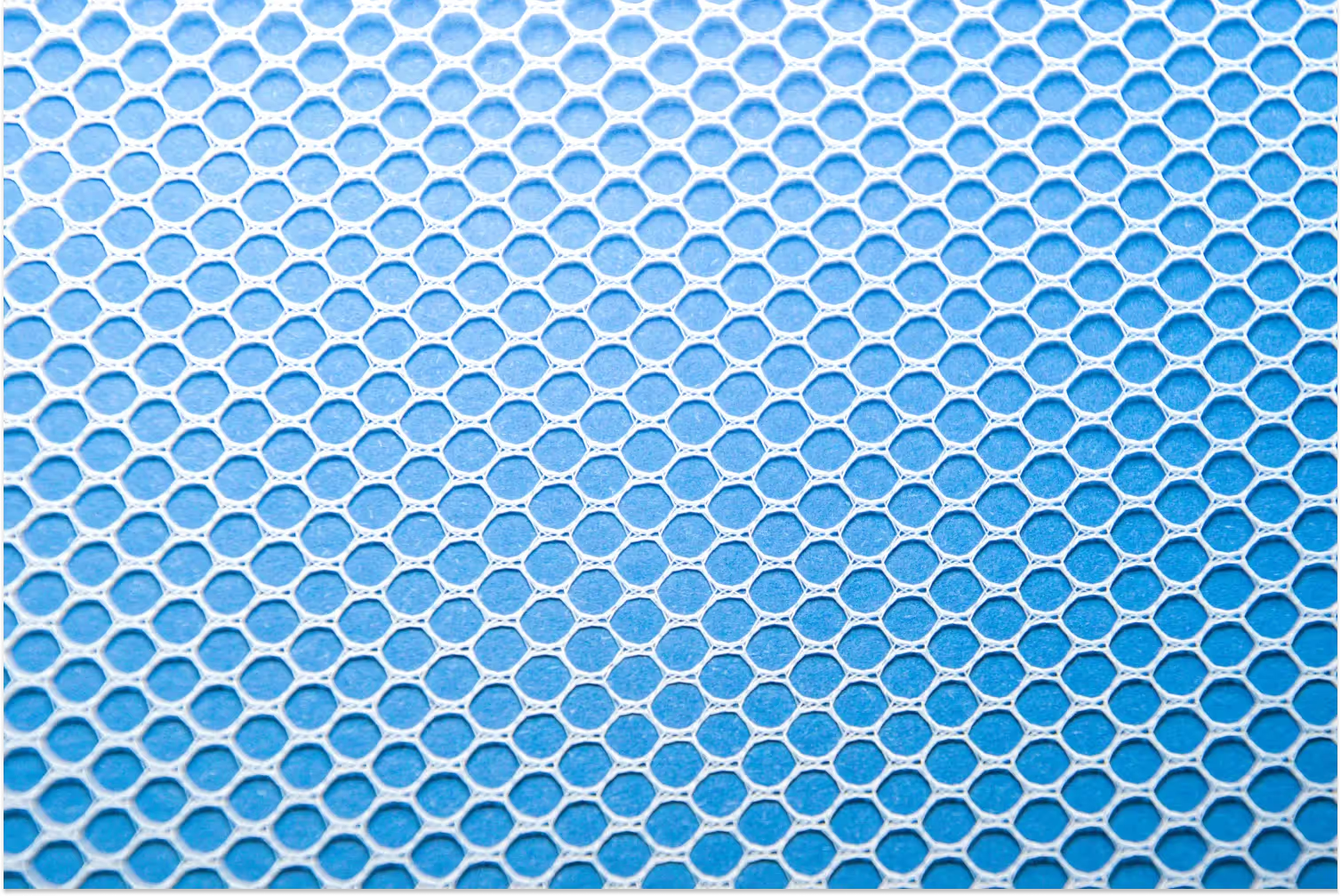
The mesh itself can be made from a variety of materials. Commonly, it is constructed from synthetic materials, like polypropylene, polyester, or expanded polytetrafluoroethylene (ePTFE).
Some meshes are absorbable, meaning they break down and are absorbed by the body over time, while others are permanent and remain in the body indefinitely. There are also biological hernia meshes derived from animal tissues, which are specially treated to be compatible with human use.
Ultimately, the choice of hernia mesh, be it synthetic or biological, depends on the specific needs of the patient and the recommendations of the medical professional overseeing the procedure. Whatever the material, the core purpose of the mesh remains consistent: to reinforce the affected area and prevent the recurrence of a hernia.
How Are Hernia Meshes Constructed?
The construction of hernia mesh is a culmination of medical engineering and design, ensuring durability and flexibility to adapt to the body's movements.
Synthetic meshes, made from materials like polypropylene, polyester, or ePTFE, are woven into sheets that can be cut and shaped according to the size and location of the hernia. These sheets often have a porous structure, allowing for tissue ingrowth, which aids in stabilizing and securing the mesh over time.
On the other hand, biological hernia meshes are derived from animal tissues, often porcine (pig) or bovine (cow) sources. These tissues undergo rigorous processing to remove any cellular components, leaving behind a collagen matrix.
This matrix is then cross-linked to enhance its strength and durability. The result is a flexible and sturdy mesh, which the body can easily incorporate.
The design and construction of hernia meshes also take into account factors like tissue integration, inflammation response, and the potential for adhesion or scar tissue formation. By understanding these factors, manufacturers aim to produce meshes that offer optimal patient outcomes.
How Are Hernia Meshes Used in Surgery?
The utilization of hernia mesh in surgeries has revolutionized the approach to hernia repairs. Once the surgeon has accessed the herniated site, they will typically push the protruding organ back to its original position. The hernia mesh is then placed over or under the weak spot, serving as a supportive barrier.
Depending on the type of hernia and its location, surgeons can opt for different surgical techniques. In a laparoscopic surgery, small incisions are made, and the mesh is positioned with the help of specialized instruments, reducing recovery time and post-operative pain.
For open surgeries, a larger incision is made, providing direct access to the hernia. The mesh is then sutured, stapled, or sometimes even glued into place.
Whichever technique is used, the mesh acts as a scaffold, promoting tissue growth around it. This ensures that the repaired area becomes stronger, drastically reducing the chances of hernia recurrence. As medical technology advances, the precision and efficacy of mesh placement continue to improve, offering patients a reliable solution to a challenging health issue.
What Are the Different Types of Hernia Mesh?
Hernia mesh is not a one-size-fits-all product; instead, there are multiple types, each designed for specific needs and types of hernias. The primary distinction is between synthetic and biological meshes.
Synthetic meshes are the most common and are made from man-made materials. They can be further classified into:
- Non-absorbable meshes: Typically made from polypropylene or polyester, they remain in the body indefinitely, providing a permanent support structure.
- Absorbable meshes: Made from materials that the body can gradually absorb, like polyglycolic acid, these meshes provide temporary support while the hernia heals, eventually breaking down and leaving the body's natural tissues to maintain the repair.
Biological meshes are derived from animal tissues (often pig or cow) and undergo processing to make them compatible with human bodies. They provide a natural scaffold for tissue integration and are usually reserved for infected fields or contaminated surgeries due to their reduced risk of infection.
What Are the Benefits and Risks of Hernia Mesh?
There are several benefits of hernia mesh. The introduction of hernia mesh in surgical practices has increased the success rate of hernia surgeries.
Meshes provide additional support, reducing the tension on the herniated site and drastically decreasing hernia recurrence rates. For many, it means fewer postoperative complications and a quicker return to daily activities.
However, as with any medical procedure, there are associated risks. In some cases, the mesh can cause adverse reactions such as infections, chronic pain, adhesions, or even mesh migration.
There have been instances where the mesh eroded into nearby organs or caused bowel obstructions. Allergic reactions to the mesh material or complications from improper placement can also occur.
Are There Alternatives to Hernia Mesh?
While hernia mesh has become a standard in hernia repair due to its efficacy in reducing recurrence rates, there are alternatives available for those who prefer or require a different approach.
Traditional hernia repair, known as herniorrhaphy, involves stitching the tissue together without using mesh. This method might be preferred in situations where infections are present or when patients have had previous complications with meshes.
Another alternative is the use of biological tissue flaps, especially in complex abdominal wall reconstructions. These procedures may have higher recurrence rates than mesh repairs, but they eliminate potential complications related to the mesh itself.
It's essential for patients to discuss these options with their healthcare provider to determine the best approach for their unique situation.

What Should Patients Know Before Hernia Surgery?
Preparation is crucial before any surgery. Patients should be well-informed about the procedure, post-operative care, and potential complications. Key points to consider include understanding the type of hernia they have, the chosen surgical approach (open or laparoscopic), and whether a mesh will be used.
It's also essential to know about the recovery time, activity restrictions, and signs of complications like infections, swelling, or chronic pain. Patients should discuss any concerns with their surgeon, including questions about the type of mesh or alternatives.
They should also be aware of potential long-term implications and the potential need for future surgeries. Ensuring a clear line of communication with healthcare providers can help ensure a successful surgery and recovery.
The Bottom Line
Hernia mesh has transformed the landscape of hernia surgeries, offering enhanced durability and reduced recurrence rates. Yet, like any medical device, it's not without its set of considerations. Weighing its benefits against potential risks and understanding alternatives ensures patients make informed decisions.
Through education and open dialogue with healthcare professionals, patients can confidently navigate their hernia repair journey. To learn more about healthcare and equip yourself for conversations such as these, head on over to Carda Health.
Source:

.avif)