Unveiling the complexities of medical procedures can be daunting, but understanding is the first step towards empowerment, helping you feel more prepared and at ease. While colorectal surgery is a common medical intervention, it can bring up questions and uncertainties.
We’re here to unravel the fundamentals of this important surgical area, covering everything from the anatomy of the colon and rectum to different types of procedures and how they contribute to improved health.
Let’s dive in.
What Are the Colon and Rectum?
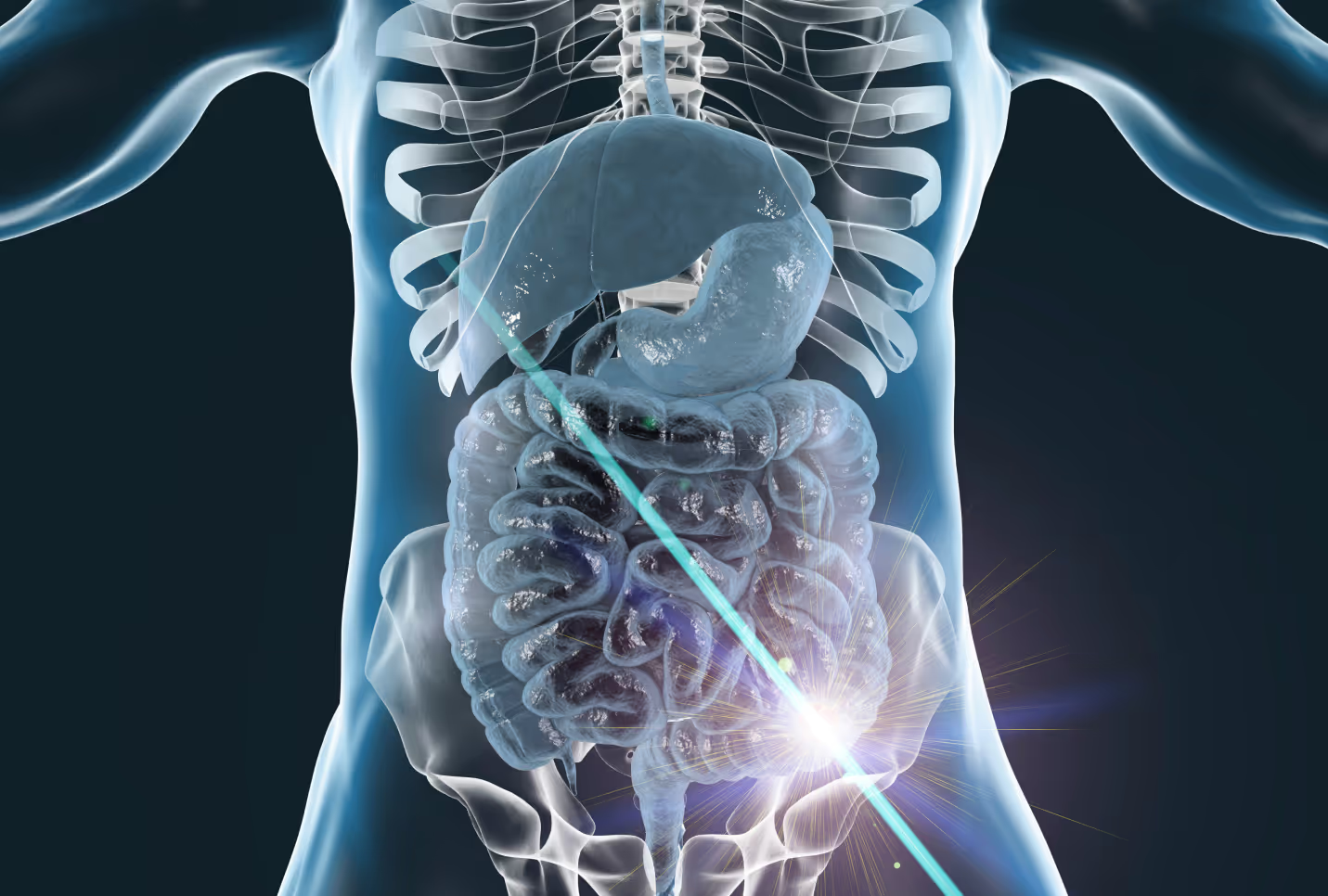
The colon and rectum are vital parts of your digestive system, playing crucial roles in processing the food you eat and expelling waste from your body. A clear understanding of these organs is essential when discussing colorectal surgery.
The colon, or the large intestine, is a tube-like organ that begins at the end of the small intestine. It continues upwards, downwards, and across the abdomen, making up most of the last part of your digestive tract.
The colon has a few key functions, one of which is to absorb water and electrolytes from digested foods. Additionally, it serves as a storage facility for waste material before it's expelled from the body.
The rectum is the final stretch of the colon, located just before the anus. Its primary function is to store feces until it's ready to be passed out of the body during a bowel movement.
Unfortunately, like all parts of the body, the colon and rectum can be affected by several conditions. One of the most common and serious of these is colorectal cancer, which is the development of cancerous growths in the colon, rectum, or appendix.
Other issues include polyps, noncancerous growths on the inner wall of the colon or rectum, and inflammatory bowel disease (IBD), which encompasses conditions like Crohn's disease and ulcerative colitis. These diseases cause chronic inflammation in the digestive tract, which can lead to a host of complications.
What Is Colorectal Surgery?
Colorectal surgery is a specialized field of medicine focusing on treatments and procedures related to disorders of the colon, rectum, and anus - encompassing a range of surgeries within this scope.
Colectomy
A colectomy is a surgical procedure designed to remove all or part of your colon. The need for a colectomy may arise from various conditions, such as colon cancer or diverticulitis, an inflammation or infection of the diverticula in the colon.
There are different types of colectomies. A partial colectomy involves removing only part of the colon, whereas a subtotal colectomy entails removing nearly all of it. In a total colectomy, the entire colon is removed. The type of colectomy a patient requires largely depends on the nature and extent of their condition.
Colostomy
A colostomy is another type of colorectal surgery. It involves creating an opening (stoma) in the abdominal wall, to which one end of the colon is attached. This allows waste to exit the body via the stoma into a colostomy bag, bypassing the rectum. A colostomy may be necessary if the colon or rectum is blocked or in cases of rectal cancer.
Colostomies can either be temporary or permanent. A temporary colostomy allows the lower part of the colon or rectum to heal after surgery, while a permanent colostomy is generally carried out when the lower part of the colon or rectum has been removed or is not functioning properly.
Rectal Surgery
Rectal surgery may be required in cases such as rectal cancer or inflammatory bowel disease. Types of rectal surgery include low anterior resection, where the upper part of the rectum is removed; abdominoperineal resection, which involves removing the rectum and anus; and transanal endoscopic microsurgery (TEM), a minimally invasive procedure to remove early-stage rectal cancer.
As with all surgeries, each type of colorectal surgery has its own benefits, risks, and recovery expectations. By adopting a healthier lifestyle and following post-operative guidelines, you can comfortably manage these surgeries and bounce back stronger.
What Are the Risks and Complications of Colorectal Surgery?
All surgical procedures, including colorectal surgeries, come with inherent risks and potential complications. It's crucial to understand these to make an informed decision about your healthcare journey.
Some common risks associated with colorectal surgery include bleeding, infection, and bowel obstruction. Postoperative bleeding is a risk with any surgery but is typically well-managed by your surgical team.
Infections, while less common due to stringent sterile techniques, can still occur and require antibiotic treatment. Bowel obstruction, or blockage of the intestines, can also happen after surgery, often due to adhesions or scar tissue formation.
Other potential complications might include changes in bowel habits, such as constipation or diarrhea, and conditions like ileus, where the intestines temporarily stop working. In more serious cases, a leak can occur at the site where the remaining parts of the colon or rectum are reconnected, which can lead to a serious infection called peritonitis.
Mitigating these risks involves teamwork between you and your healthcare providers. Open communication is key — always ensure your surgeon knows your medical history and current health status. They can then provide personalized guidance to minimize potential risks.
How Can You Prepare for and Recover From Colorectal Surgery?
Following the guidelines of your healthcare provider and taking specific steps regarding your diet, activity level, and rest can help you prepare for and recover from colorectal surgery.
Diet and Nutrition
Preparing for colorectal surgery often involves following a specific diet. Prior to surgery, you may be asked to follow a low-residue or clear liquid diet.
Post-surgery, it's important to reintroduce food gradually, starting with liquids and progressing to solid foods. It's generally recommended to have smaller, more frequent meals and to consume a diet high in fiber once tolerated to promote bowel regularity.
Staying hydrated is crucial, and you might need to avoid certain foods that could lead to gas and bloating. It can be helpful to consult with a registered dietitian who can provide personalized advice based on your condition and surgery type.
Physical Activity
Movement is a critical part of the recovery process after colorectal surgery. Simple activities like walking can help to prevent complications such as blood clots and pneumonia and help in waking up your digestive system after surgery.
While it's important to stay active, remember to balance activity with adequate rest. Pushing yourself too hard too soon can delay your recovery.
Always follow the guidance of your clinical exercise physiologist or physiotherapist, and remember that at Carda Health, we're here to guide you through your rehabilitation journey, providing a comfortable and personalized approach to your recovery.
By adhering to these guidelines and maintaining an open line of communication with your healthcare team, you can prepare for and recover from colorectal surgery successfully. Always remember that at Carda Health, your comfort and well-being are our priority.
What Does Follow-Up Care Look Like After Colorectal Surgery?
Following colorectal surgery, thorough and continuous follow-up care is essential to monitor healing, manage any post-operative symptoms, and facilitate a smooth return to daily activities.
Immediately after surgery, you will typically remain in the hospital for several days so medical staff can monitor your recovery, manage pain, and ensure that your digestive system is functioning correctly. Once discharged, you will need to schedule follow-up appointments with your surgeon to check your surgical site and discuss any concerns or symptoms.
Additionally, you may require further diagnostic tests, such as blood tests or imaging studies, to ensure your body is healing properly and to monitor for any signs of recurrent disease, especially in cases of cancer.
For patients who have undergone a colostomy, follow-up care will also involve education on how to manage the colostomy, including learning how to change the bag, recognize signs of infection, and address any potential issues that may arise. It can be quite a change, but with the right guidance and a bit of practice, most people find that they can manage it successfully.
Remember, follow-up care is a team effort. Regular check-ins with your healthcare team, including doctors, nurses, and exercise physiologists, will ensure a smoother recovery and a quicker return to an active lifestyle.
The Bottom Line
Navigating the path to recovery after colorectal surgery may seem daunting, but with the right information and support, it can be a manageable process. It's essential to understand not only what the surgery involves but also what you can expect during recovery and how you can actively participate in your healing process.
Remember, colorectal surgery is a significant step towards a healthier, more active life. With a clinically-proven approach and the comprehensive support of the Carda Health care team, you can be well on your way to reclaiming control of your health.
At Carda Health, our approach is not about quick fixes but about sustainable and active living post your cardiac event. By taking a holistic approach to wellness, our expert clinical physiologists can help you feel more empowered in managing your overall health.
By focusing on your health, improving your symptoms, and adopting a healthier lifestyle, you can live a more active life. Remember, we're here to support you every step of the way.
Sources:
Digestive System: Function, Organs & Anatomy | Cleveland Clinic
Inflammatory bowel disease (IBD) - Symptoms and causes | Mayo Clinic

.avif)